 The Brian Lehrer Show
The Brian Lehrer Show
The Latest on Masks and COVID Vaccines for Kids
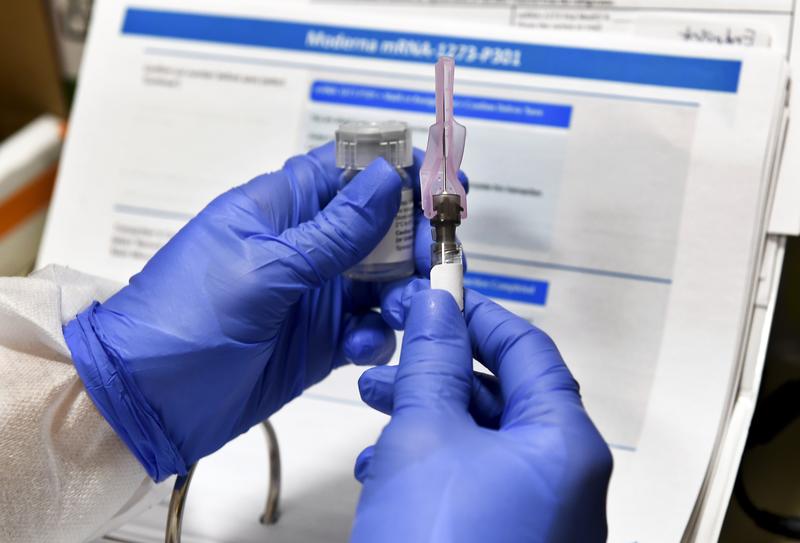
( Hans Pennink) / AP Images )
[music]
Brian Lehrer: Brian Lehrer on WNYC. Did you hear that yesterday Moderna announced that its COVID-19 vaccine was 100% effective in a study of adolescents ages 12 to 17? The company said it plans to ask the FDA to expand the emergency use of its COVID vaccine for that age group early next month 12 to 17.
If approved, the number of shots available to middle and high school students would dramatically increase ahead of the next school year. As we know, Mayor de Blasio and Governor Murphy have both announced that public schools will fully reopen in the fall with no remote option. There still isn't anything available for kids under 12, leaving them more vulnerable.
Another COVID headline yesterday, a milestone, half of all American adults are now fully vaccinated, according to government figures. With that progress and more things reopening but still all these uncertainties about kids, joining us to discuss the latest science and what it might mean for your family is Dr. Leana Wen, emergency physician, professor at George Washington University, contributing columnist for The Washington Post, and a CNN medical analyst.
Her latest opinion piece with The Washington Post is called, The Pandemic Isn't Over, Especially for Our Children. She's also the former Baltimore Health Commissioner and author of the forthcoming book Lifelines: A Doctor's Journey in the Fight for Public Health. Dr. Wen, always great to have you. Welcome back to WNYC.
Dr. Leana Wen: Thank you, Brian. Great to join you.
Brian Lehrer: In your Washington Post column released yesterday, you mentioned the pediatric infections or you mentioned that pediatric infections are now 24% of new weekly cases which is up from 14% that's up substantially since the beginning of the pandemic. Why do you think that is?
Dr. Leana Wen: Part of it is the great news, and I'm so glad, Brian, to be talking to you about good news for once because, throughout the pandemic, we've given bad news. Now, the feeling of foreboding has been replaced by one of optimism. We have vaccinated over 50% now fully of the adult population. In some ways, it's understandable that children constitute a higher proportion of the number of new infections because so many adults now have immunity.
I think though that I wrote this article because I wanted to point out that the pandemic is not over for our children. That actually a Washington Post analysis done in the last few days found that when you take out the people who are vaccinated, the risk to those who are unvaccinated is about the same as it was back in January, during the peak of the pandemic.
When we think about adults who are unvaccinated but also very specifically our children, they are still at risk. Now, children tend to get much less severely ill than adults do, but as a parent of two young kids, I am worried that so many people seem to have taken the CDC's latest guidance as a sign that we now can go around maskless even if you're unvaccinated and I worry about my children now actually being exposed to higher risk because if they're going to be in grocery stores or in pharmacies and are surrounded by unvaccinated unmasked people, they are at risk. I hope that we as a society are sensitive to that.
Brian Lehrer: You also wrote that the risk of hospitalization among the unvaccinated has more than doubled compared with January, so that makes common sense based on what you were just highlighting. As you also wrote in your column, COVID-19 remains a real concern for many including families with young kids. As you know, Dr. Wen, a lot of parents have concerns about vaccinating their kids. Let's get into some of those concerns. As you address in the column, "Children are unlikely to become seriously ill from the virus," so why should parents vaccinate their kids in your professional opinion?
Dr. Leana Wen: It is true that children tend to be much less severely ill than adults, but let's not forget that kids have become ill. We're talking about over 10,000 hospitalizations that have involved children in this pandemic. More than 3,000 children according to the CDC have had this multi-system inflammatory syndrome that involves inflammation of multiple organs.
More than 300 children have died of COVID during the pandemic, and so I would take issue with those who say that children just don't get ill because that's not true, children have become sick from coronavirus. We also know that children have been severely affected because of COVID because of school closures because kids have not been able to see their friends and participate in extracurriculars and sports the way that they have before.
I think a lot of families are eager to return to normal as a family and as long as their children are not yet protected from using the vaccine, they don't feel ready to engage fully the way that they would when their kids are vaccinated. Now, we know that the Pfizer-BioNTech vaccine is authorized for adolescents 12 and older. Moderna, you had mentioned earlier, there is now good news from their clinical trials too.
For all the parents of 12-year-olds and above who now are getting vaccinated, I know they are breathing a deep sigh of relief that their kids can now return to sleepovers and birthday parties, and hopefully, will have a very normal next school year. I certainly cannot wait until the time that kids in younger age groups-- I have kids one and three and a half. I can't wait for them to also be eligible for vaccination, and I'll be first in line when that occurs.
Brian Lehrer: We have to also acknowledge another headline and that is that the CDC is looking into possible links between a heart problem called myocarditis and COVID vaccines in a small number of young people. It could still be unrelated because this condition does occur. I don't think they found yet an elevated number total in the population, but some have happened close to the date of vaccinations. Although the CDC hasn't released the exact number of cases, NBC News identified at least 55 suspected cases nationwide. In your opinion, what's going on here?
Dr. Leana Wen: I think this deserves an investigation. I actually think that we should look at what happened with Johnson & Johnson, with the CDC and the FDA using a real abundance of caution approach. Even when the case count was something like one in a million potential cases of this rare blood clotting disorder, they shut down. The distribution of the Johnson & Johnson vaccine, that's how cautious they are being.
At the moment, when we look at the percentage of people with myocarditis, this inflammation of the heart muscle, for people in the general population versus people who have received the vaccine, there's no difference. Right now, there's not enough even for us to look for correlation much less causation. I do think that they're using another abundance of caution approach here and being very transparent about the investigation which is important. We certainly need to look into this.
I am not concerned about this and again, would really urge for people to wait for the results of the investigation and to know that these vaccines have been now shown in well over a hundred million people here in the US, the mRNA vaccines, the Pfizer, Moderna vaccines have been shown in so many millions of Americans to be safe and very, very effective. This is the reason why we're seeing this dramatic decline in the number of infections, hospitalizations, and deaths because of the extraordinary benefit of these vaccines.
Brian Lehrer: What about the effect of the vaccine on hormones in young people? We've had a number of callers asking about vaccines affecting fertility in young women and the beginning of menstruation in girls reaching puberty. What do you say to those with these concerns?
Dr. Leana Wen: Yes, I have heard them as well, and I think it's important for us to acknowledge a concern that some people have which is that, we don't know the long-term effects of these vaccines. I actually think we should be honest and acknowledge them. We don't know, how could we possibly know considering that these vaccines have not been around for many years. We can't say for certain that there isn't going to be some effect 20 years down the line.
However, here's what we do know, we know that for all the other vaccines that we have against polio, measles, mumps, rubella, et cetera, that we see for all these other vaccines that have been around for many dozens of years that we do not see side effects of these vaccines beyond the six-week mark. Is it, in theory, possible that there may be some kind of long-term side effects many years down the line? It's purely a hypothetical, but of course, we can't rule it out.
However, there is no scientific or physiologic reason for us to believe that that's the case and that's what I would say for individuals concerned about fertility, maybe there could be an effect on menstruation in the short term but there's no reason for us to think at all that there's some impact on fertility years later.
I think people really need to weigh whatever theoretical, hypothetical risk there is that we can't disprove because you can't disprove a negative but you have to weigh that against the real benefit of preventing a deadly disease that has so far claimed the lives of nearly 600,000 Americans.
Brian Lehrer: If you're just joining us, listeners, it's our latest visit from Dr. Leana Wen, former Baltimore Health Commissioner, Washington Post columnist, and CNN medical contributor, and George Washington University professor of medicine. Let me go on with you to the school reopening plan. New York City and New Jersey both now planning to be fully in-person in the fall with no remote option, does a full reopening with no remote learning option seem like a good idea to you?
Dr. Leana Wen: Yes. I believe that we should absolutely be able to return back to full in-person learning come the fall for several reasons. One is that we already have the lowest infection rates that we've had in nearly a year. I would expect that the infection rates are going to fall even more over the course of the summer as more people are getting vaccinated and especially our adolescents are now getting vaccinated as well.
I also think that because our staff and teachers have had now a humble opportunity to be vaccinated themselves, that also reduces the risk to teachers which is something that I've been very concerned about in the beginning. The reason why I was very concerned about some of the initial plans for reopening schools in the middle of the surge, I was very concerned about the wellbeing of teachers and staff who worked in our schools.
I also think that come to fall, we're going to have at least high school-age students who can all be vaccinated. I think there should be conversations about whether vaccination should even be required in these students, because as we're seeing in the case of colleges now more than 400 colleges and universities are requiring vaccinations come to fall, they will be able to have a essentially totally normal pre-pandemic experience without masks or distancing.
I think a lot of schools will really want to do that as well and so in consideration of whether the COVID vaccine can be added to the required list of childhood immunizations, I hope is a conversation that will be heard over time.
Brian Lehrer: Even if that were to happen, there would be mixed populations of vaccinated and unvaccinated in the lower grades at best. I'm curious if under those circumstances, do you have an opinion on what that should look like? Like masks will be required of the kids in schools in New York City in the fall as of now and the CDC still has those guidelines of three feet between students in the lower grade, six feet in the upper, which is scrambling the brains of school administrators, because they don't have enough classrooms to have kids at that small numbers and not enough teachers.
Do you think that's the way to go in the population of children that will be a mix of vaccinated and unvaccinated even 12 plus in many cases and how do they do that?
Dr. Leana Wen: It's a great question and I think these are the subjects that the CDC should be tackling. I'm sure they are. I hope they come out with guidelines pretty soon, that look at two key areas. One is, can we have some kind of differentiation based on the number of cases? If we actually have very, very low infection rates in some parts of the country come the fall, because there are some areas that will be able to achieve herd immunity. If we're able to get to very low levels, maybe we don't need distancing and masking in our schools.
Something else that they should be looking at is we keep on talking about layered mitigation. Understanding that masks are a layer, vaccination is another layer, testing is another layer as well. If you have vaccination plus testing, can that replace masks and distancing, especially at lower levels of infections?
I do think then it's going to be challenging come the fall because there is some concern that there could be a resurgence of coronavirus come the winter months when it gets colder, when this is a winter respiratory virus and there are parts of the country that have not reached very high rates of vaccination and so what are we going to face come the winter?
What happens if students start having a cough and fever? What kind of testing protocol is available at that point? I think there are lots of unanswered questions that the CDC would do well to start providing some interim guidance. Especially as, of course, schools are planning come the fall already.
Brian Lehrer: We have 30 seconds left. Do you have an opinion yet as to whether all the vaccinated people are going to need boosters sometime this fall?
Dr. Leana Wen: I think it's possible, but I also don't want us to speculate on this just yet. I think it's important for the research to continue for us to be really tracking the rate of breakthrough infections among vaccinated people to see when it is that people may need boosters or not. We also have to be careful that even talking about boosters is a major reason why those who are hesitant about vaccines may not be getting the vaccine. We really need to be careful about how we're framing this issue and not speculating until we have the science and evidence.
Brian Lehrer: Dr. Leana Wen, science-based emergency physician, Professor at George Washington University, contributing columnist for the Washington Post. Her columns have been having a lot of impact on the public dialogue, and a CNN medical analyst. Her latest Washington Post column is called The Pandemic Isn't Over, Especially for Children.
She's the former Baltimore Health Commissioner and author of the forthcoming book, Lifelines: A Doctor's Journey in the Fight for Public Health. DR. Wen, we always appreciate it. Thank you so so much.
Dr. Leana Wen: Thank you very much, Brian.
Brian Lehrer: Brian Lehrer on WNYC, much more to come.
Copyright © 2021 New York Public Radio. All rights reserved. Visit our website terms of use at www.wnyc.org for further information.
New York Public Radio transcripts are created on a rush deadline, often by contractors. This text may not be in its final form and may be updated or revised in the future. Accuracy and availability may vary. The authoritative record of New York Public Radio’s programming is the audio record.